There are many types of brain imaging we can get in patients presenting with stroke.
- CT head without contrast
- CT angiogram of head and neck
- Multiphase CT
- CT perfusion
- MRI with diffusion-weighted imaging
- Fluid attenuated inversion recovery (FLAIR) – T2 weighted sequences
- Susceptibility weighted MR
- MR angiograms
- Perfusion weighted imaging
It’s good to know what the different types are and why we’d use them, but realistically we’d only probably get the bolded ones above.
CT scanning
CT head without contrast is generally ordered to eliminate the possibility of an intracranial hemorrhage. You won’t see the signs of stroke until much later. However, you can see a hyperdense MCA sign sometimes.


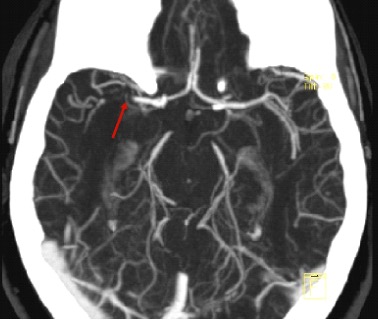
CT angiogram is useful in identifying LVO to select patients who may be candidates for endovascular therapy. This could be useful in patients with a high NIHSS = 7-10 to evaluate for LVO and 11-14 may require thrombectomy. It helps determine how accessible the clot is. Not all centers do these routinely on all stroke patients. More than the risk of renal injury (0.04%) is the risk of allergy.
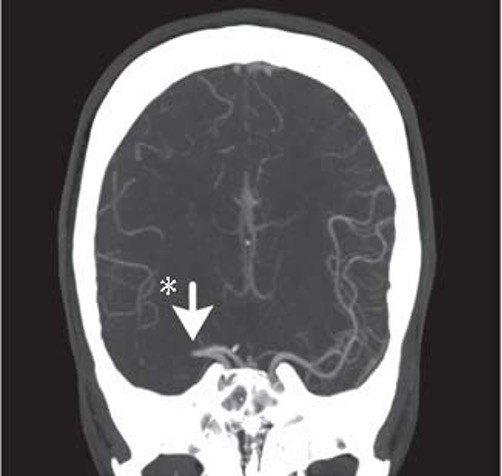
Multiphase CTA has three sets of pictures: an arterial, venous (8s later) and late venous phase (16s later) to check for collateral circulation, important in prognosis.
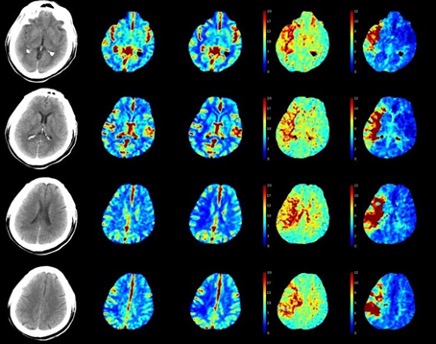
CT perfusion quantifies cerebral blood volume (CBF) mean transit time for blood flow through brain tissue. This is done through a repeated series of scans through the anterior circulation over 1 minute after a bolus of contrast is administered. We watch the bolus go through the vascular territory. This is useful to identify alterations in cerebral blood flow to distinguish the infarct from the penumbra. It is 6x more radiation, needs to be interpreted by software to get color coded, and may result in some false positives and negatives. Useful for patients who are 6-24 hours from LKW to see if they are a candidate for a thrombectomy.
MRI scanning
MRI with diffusion-weighted imaging is the most accurate for ischemic stroke usually within minutes of injury by detecting cytotoxic edema due to ischemia. It can miss an acute infarct in 7% of the patients: eg, posterior circulation, small brainstem strokes. Changes appear in the first few hours after stroke and is useful for unknown onset time (eg, >4.5h or wake-up strokes). The AHA approves tPA when DW-MRI is smaller than 1/3 of the MCA territory and no signal change on FLAIR. All stroke patients get an MRI within 24 hours.
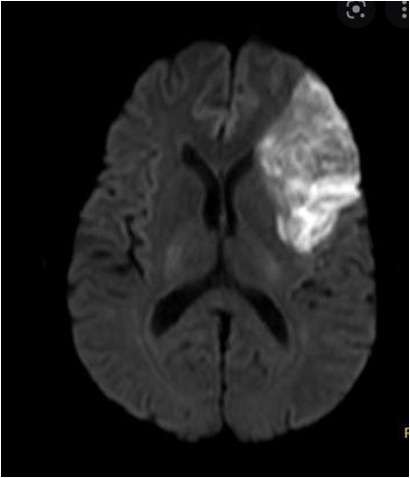
T2 weighted sequences / Fluid attenuated inversion recovery (FLAIR) can diagnose sub-acute IS within 3-8h of symptoms, old strokes and SAH (but not as good as plain brain). Comparing the DWI with FLAIR is useful in determining if a wake-up stroke is a TNK candidate: +DWI but -FLAIR. FLAIR suppresses fluid on the images to make edema, old infarcts and glimpses more obvious. FLAIR lags DWI by hours.
Susceptibility-weighted imaging uses the magnetic properties of deoxygenated Hgb to identify intravascular thrombus vs calcification.
MR angiograms can find occlusions and stenoses, evaluate the cranial circulation without the use of IV contrast. This is useful for identifying secondary causes of ICH like vascular abnormalities (aneurysms, AVMs). The time-of-flight 3D reconstructions are affected by motion artifact, by the patient but even blood flow. They can overestimate vessel stenosis.
Perfusion weighted imaging (PWI) depicts areas with reduced cerebral blood flow. A DWI-PWI mismatch can estimate an area of brain tissue at risk of infarction (penumbra) if blood flow not restored.
Gradient-recalled echo (GRE) MRI diagnoses acute ICH and detects chronic ICH.
You must be logged in to post a comment.