Here’s what you need to get out of this section.
- Review the diagram below and understand the process.
- Review the thrombolysis timeline metrics
- Be able to screen for stroke (BEFAST) and recognize large vessel occlusions (LVO) that may benefit from endovascular therapy.
timeliness leads to better outcomes
The diagram below shows our ED and Neurology workflow for patients presenting with stroke-like symptoms. Before delving into it deeply, it’s important to know why we do what we do.

Early recognition and treatment of stroke patients is critical for improving patient outcomes. Brain tissue is incredibly sensitive to ischemia, with damage occurring in as little as 10 seconds. Each minute without reperfusion destroys 1.9 million neurons. Our primary goals in managing stroke are to rapidly restore blood flow to the affected brain regions, preventing further neuronal damage, and to minimize the risk of recurrence.
stroke is a leading cause of US morbidity and mortality
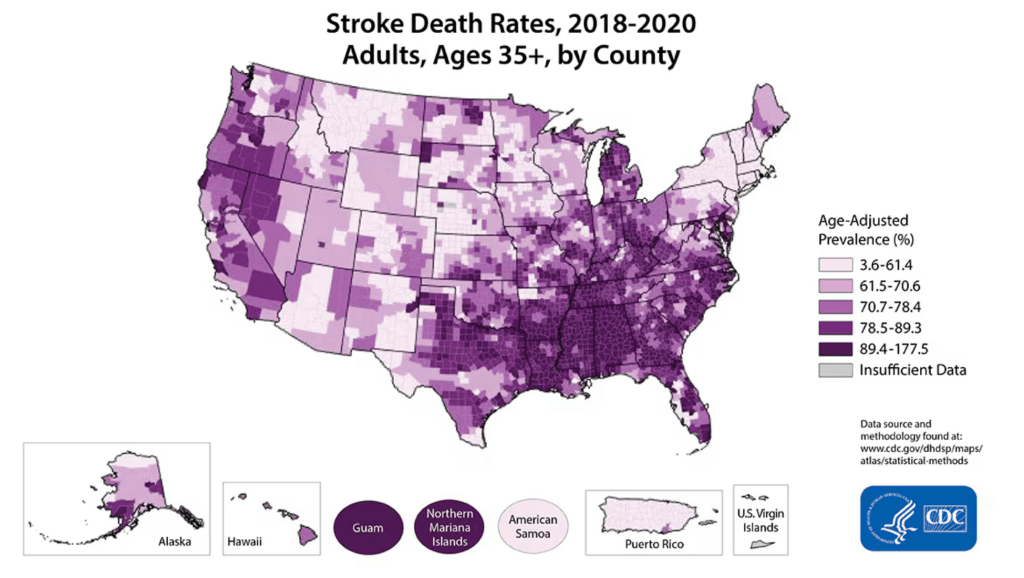
Someone has a stroke every 40 seconds in the US, that’s 795,000 strokes (87% are ischemic, 23% are recurrent). 240,000 people have TIA’s each year. Stroke is the 5th leading cause of death in the US with 162,980 US deaths in 2021. This has increased 8.4% from 2011. The number of strokes increased 26.3%. CDC Stroke Facts
the ED plays an important role in the care of stroke patients
The Emergency Department (ED) plays a pivotal role as one of the initial points of contact for stroke patients. An organized approach to stroke care is essential, enabling coordinated efforts across all healthcare teams. Our performance is measured against several benchmarks to ensure we achieve the best possible outcomes.
| Therapy | Metric | Goal | Recognition Target |
|---|---|---|---|
| Thrombolysis | Door-to-MD-Evaluation | ≤ 10 min | |
| Door-to-Lab/CT-Order & NIHSS | ≤ 10 min | ||
| Door-to-Stroke-Team-Page | ≤ 15 min | ||
| Door-to-initiate-CT-scan | ≤ 25 min | ||
| Door-to-CT-read | ≤ 45 min | ||
| Door-to-Lab-Review (Labs Complete) | ≤ 45 min | ||
| Door-to-tPA-Checklist | ≤ 45 min | ||
| Door-to-TNK | ≤ 60 min | Honor Roll: 75% of the time Honor Roll Elite: 85% Honor Roll Elite Plus: ≤45m 75% of the time and 30m 50% of the time | |
| Endovascular Therapy | Arrival-in-lab to puncture | ≤ 30 min | |
| Puncture-to-Recanalization (TICI 2B or higher) | ≤ 60 min | ||
| Arrival to Recanalization (TICI 2B or higher) | ≤ 120 min | ||
| Door-to-First Pass (ED/Direct Arrival) | ≤ 90 min | ||
| Door-to-First Pass (Transfers) | ≤ 60 min | Honor Roll Advanced Therapy: 50% of the time |
For comprehensive guidelines and metrics specific to Rush University Medical Center, please refer to the Stroke section in Department Links on Epic or on the Comprehensive Stroke Center’s page on Inside Rush
stroke center recognition helps improve care
Achieving stroke center recognition not only confers prestige but also ensures that our institution has the necessary resources to deliver the highest quality care. The American Heart Association (AHA) and American Stroke Association (ASA) have established several time-based best practices that we’ve incorporated into our response protocols.
- EMS notification to the receiving hospital when stroke is recognized in the field
- Stroke toolkit containing rapid triage protocol, clinical decision support, stroke-specific order sets, guidelines, hospital-specific algorithms, critical pathways, NIHSS
- Rapid triage protocol and stroke team notification
- Single call activation of the entire stroke team by the ED
- Direct to CT: Triage of eligible stroke patients directly from ED triage to the CT scanner, bypassing the ED bed
- Timely imaging: Rapid acquisition (within 25 minutes) and interpretation (within 45 minutes) of brain imaging
- Rapid lab testing (within 30 minutes), including glucose and coags.
- Pre-Mix rt-PA as soon as the patient is recognized as a potential rt-PA candidate, even before brain imaging is completed. The use of TNK (tenecteplase) has made this quicker.
- Prompt IV rtPA administration: Rapid access and administration of IV rt-PA, with consideration of initial bolus being given on the CT table.
- Team-based approach with an interdisciplinary collaborative stroke team.
- Performance tracking: Monitor stroke performance metrics with feedback mechanisms for continuous improvement.
There are several different level of stroke centers. We are a comprehensive stroke center (CSC).
- Acute Stroke Ready Hospital: (ASR): Able to initiate tissue plasminogen activator (tPA) prior to transfer to a higher-level stroke center
- Primary Stroke Center (PSC): Have protocols and specific care pathways for patients with stroke
- Thrombectomy-Capable Stroke Center (TSC): Able to initiate tPA and provide endovascular treatment
- Comprehensive Stroke Center (CSC): Can initiate tPA, provide endovascular surgery, and neurocritical care with stroke-specific protocols and care pathways.
address the bottlenecks
We have addressed several bottlenecks to timely stroke care. It takes the entire team working like clockwork to ensure all the pieces fall into place at the right times.
- Early recognition of patients who are in the treatment window for IV thrombolysis or endovascular mechanical thrombectomy of large vessel occlusions. This can be done by pre-hospital personnel, the greet and triage nurses or physicians.
- Quick registration of patients to generate an MRN to facilitate the ordering of tests and transmission of images. Our registration / finance staff have been amazing in getting this done quickly. So much relies on having the patient “in the computer.”
- Quick ordering of stroke labs and images using the ED Acute Stroke order set to ensure labs and images are tied to MRN’s for quicker review. The ED physicians (or potentially charge nurse) should do this as soon as the patient is register. You can do this from the computers in the CT scanner suite.
- Order CT angiograms of the head and neck quickly. This requires that patient’s have IV’s and often a point-of-care creatinine values (in those who we may be worried about renal disease) completed. This often happens in the CT scanning suite. These orders are now included with the initial orders (see #3).
- Make the decision on whether to give or not give thrombolytics quickly. We have established a “stroke huddle” when the patient comes back from CT to work through these as a team (Neuro and ED). There are several things that can slow this step down:
- Inability to talk with the patient (aphasia)
- Inability to control blood pressure (despite medications)
- Inability to get informed consent in a timely fashion
- Uncertainty about patient contraindications to thrombolytics
early recognition begins with a validated screening tool
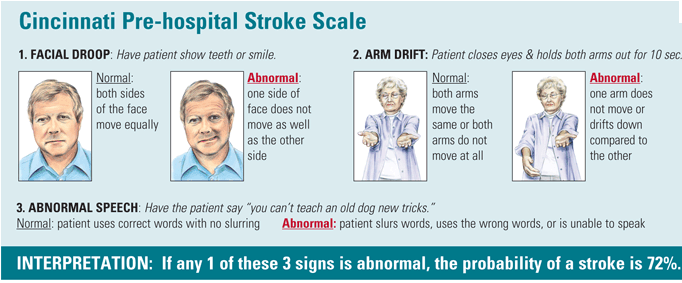
Across the country, several different scales are used for the early recognition of stroke: California Prehospital Stroke Screen, Los Angeles, Cincinnati, and abbreviated NIH Stroke Screens like NIHSS-8 and NIHSS-5. They have pretty good sensitivity and specificity and picking up stroke.
Cincinnati Pre-Hospital Criteria
Chicago EMS uses the Cincinnati criteria.
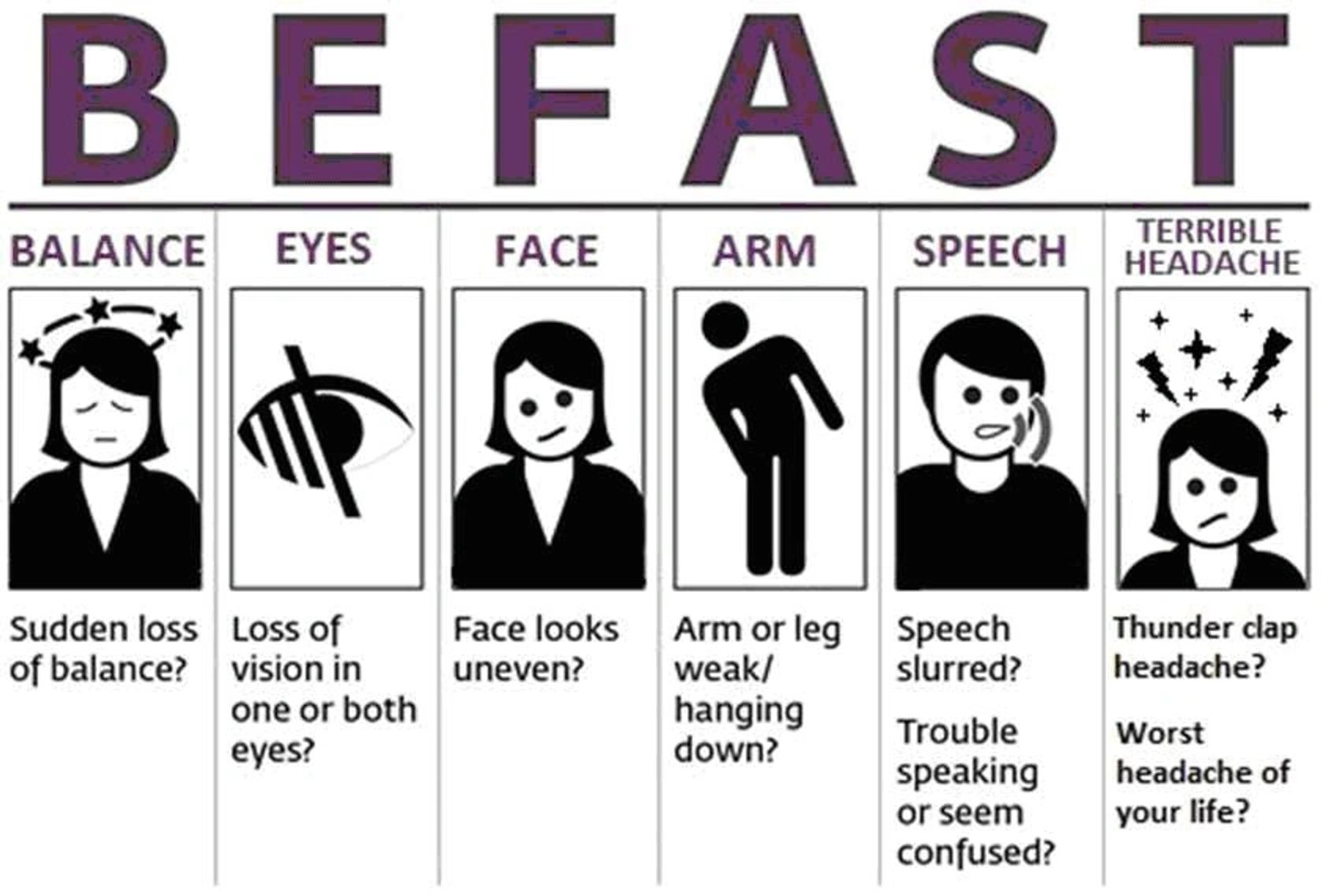
BEFAST Screening
In triage, we use the BEFAST screening tool.
LVO Screening (FANG)
Another important condition to screen for are large vessel occlusions. This disease process is potentially amenable to endovascular mechanical thrombectomy (MT). These can spell FANG (I don’t know, maybe Dracula wants to bite into your large vessel with his fang).
- Field cuts (visual field cuts)
- Aphasia
- Neglect (hemi-neglect)
- Gaze deviation
get the patient to the right place upon arrival

Patients can arrive to the ED either by ambulance (after calling 911) or on their own.
- EMS can screen for stroke, call in to Rush, and then we can activate the acute stroke code even before arrival.
- Those who walk in are seen initially by the greet nurse (who can screen using BEFAST and LVO and activate the strong code) or send to triage (where they can also be screened). If there’s doubt, a physician is called to triage to make the decision whether to activate stroke.
- If the patient doesn’t meet acute stroke code criteria, then we can consult neurology via the non-acute pager.
once recognized, they go straight to CT
Identified patients are quickly registered (to get an MRN to facilitate the ordering of tests), the acute stroke team is notified, the ED places the ED Acute Stroke Order Set and the patient is taken directly to the CT suite. The Neurology team will meet the patient at the CT scanner and do their history and exam. The CT Head is primarily used to rule-out any intracerebral hemorrhage or other contra-indications for thrombolysis.

If there’s concern for potential large vessel occlusion and it won’t delay giving TNK (meaning, the patient has an IV already), the CT angiograms are done. If it would cause a delay, the patient can be brought back to the ED, TNK given, and then be brought back to the CT scanner.
once back in the ED, time for a stroke huddle
The stroke huddle allows all involved (nurses, neurologists, ED physicians, pharmacists) to get on the same page on three decisions:
- The decision to give TNK or not
- Need for additional imaging
- Ultimate disposition of the patient.
You must be logged in to post a comment.