Our goal in diagnosing acute coronary syndromes is not to diagnose ST-elevations but coronary artery occlusions leading to myocardial infarction (OMI). In the past, we diagnosed heart attacks by looking for Q-waves, thus missing all the ST-elevations. EKG manifestations only are a marker for what’s going on underneath. Within the broad bucket of NSTEMI, 25% of these are due to occlusion. So, what are all the other markers for coronary occlusion that we can see?
According to the 2014, ACC which NSTEMI’s should go to the cardiac cath lab?
NSTEMI’s that would benefit from reperfusion Tx include:
- refractory CP
- recurrent CP
- sustained dysrhythmia or
- hemodynamically unstable.
Which additional patients do the Europeans send to the cath lab?
The Europeans (2020) add:
- heart failure,
- STE in AVR & V1 with diffuse STD, or
- delta troponin.
Everyone else gets delayed invasive therapy (24-72 hours later) including the high risk patients. On average,
- STEMI = 41 min to cath
- NSTEMI = 437 minutes to cath
But 38% of these NSTEMI’s were OMI. Pendel Meyers, J Emerg Med 2021
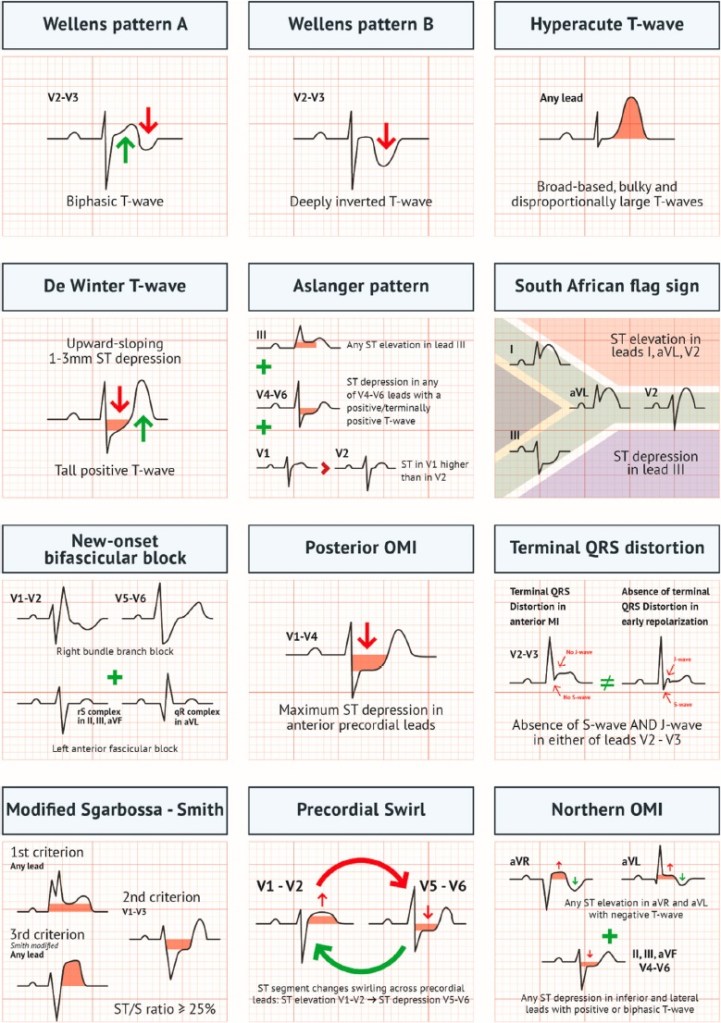
Along with STEMI, what are the five STEMI equivalents (together known as OMI) we should look for on ECG’s?
- STEMI
- hyperacute T waves
- Wellens A & B
- Posterior MI
- RV MI
- de Winter T-waves
ECG findings can change with time. Don’t forget the importance of serial ECG’s in chest pain.
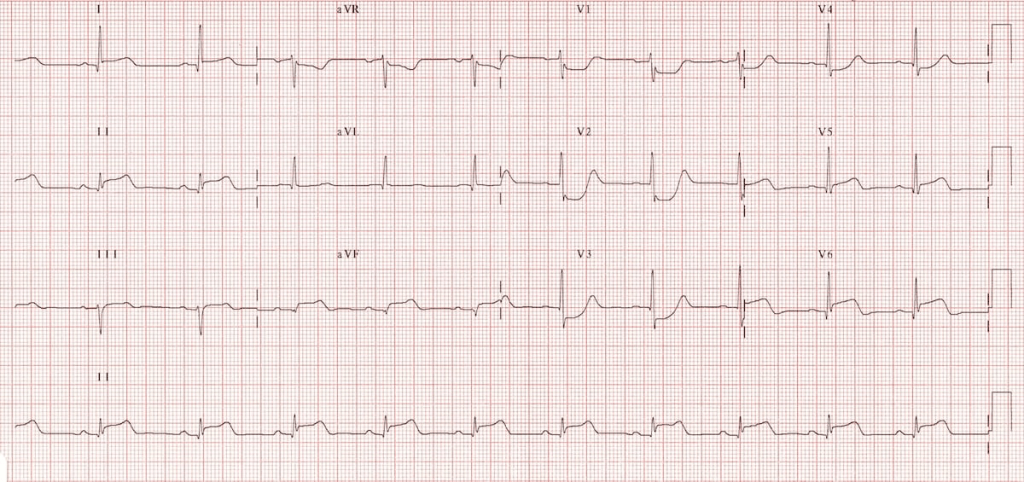
Name the STEMI Equivalent
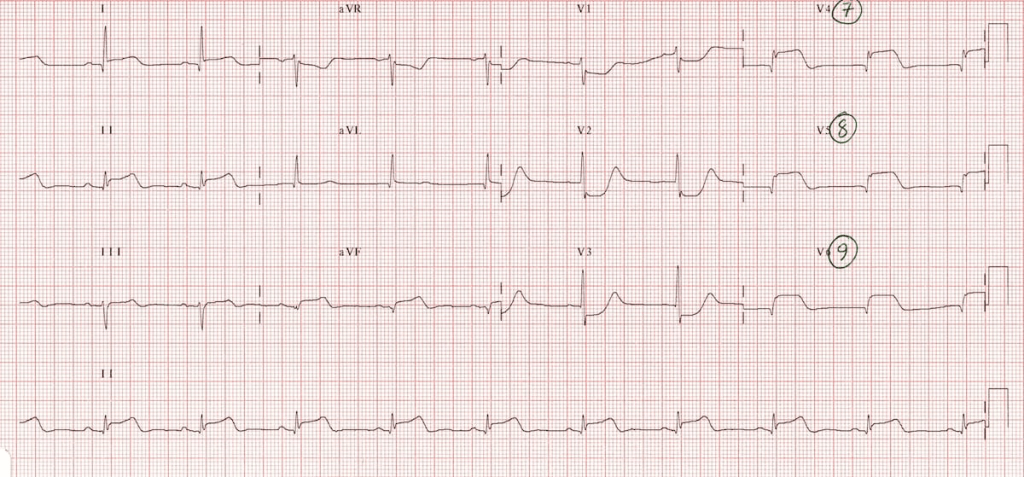
EKG 01

Answer 01
de Winters T-waves
ECG Diagnostic criteria:
- Tall, prominent, symmetrical T waves in the precordial leads
- Upsloping ST segment depression > 1mm at the J point in the precordial leads
- Absence of ST elevation in the precordial leads
- Reciprocal ST segment elevation (0.5mm – 1mm) in aVR
- Typical STEMI morphology may precede or follow the De Winter pattern
EKG 02
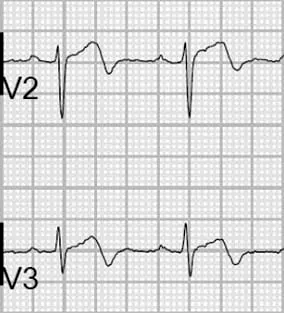
Answer 02
Wellens Type A
- biphasic T waves in the precordial leads (v2 – v3),
- 25% of cases
- biphasic T waves in V2/V3
EKG 03
Answer 03
Posterior MI
Get posterior leads whenever you are suspecting posterior MI: V7, V8, V9
- easily missed due to absence of STE, usu occlusion of RCA or LCx, so may present with inferior MI (RCA) and ant-septal STD (V1-V3).
- Need to get a posterior ECG with V7, V8 and V9, but the absence of STE in posterior leads does not exclude a posterior MI
- Implication: LCx or RCA occlusion
EKG 04
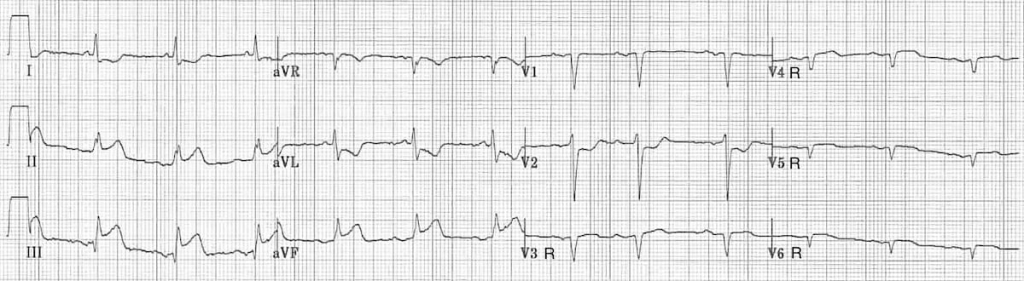
Answer 04
right ventricular MI
- one third of inferior MI’s have RV involvement
- treatment is IVF and inotropes; preload reducers can cause hypotension.
- criteria (looks like V1 may be the transition between STE and STD, so it may be up or flat); also look for the associated inferior MI — but the key is STE in V1
- ST elevation in V1
- ST elevation in V1 and ST depression in V2 (highly specific for RV infarction)
- Isoelectric ST segment in V1 with marked ST depression in V2
- ST elevation in III > II
EKG 05

Answer 05
Wellens Type B
- 75% of all cases
- deep symmetrical T wave inversion in V2/V3
- high grade LAD lesion
- present when pain free, but disappears with chest pain (pseudonormalization) — serial ECG’s are important in all patients with chest pain
EKG 06

Answer 06
Hyperacute T-waves
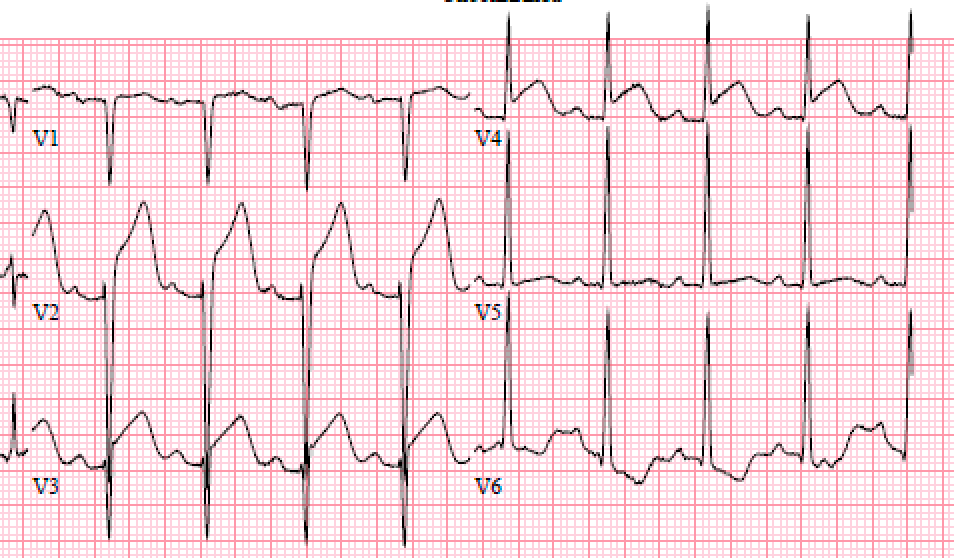
Here’s the same EKG 2 hours later.
- the above ECG’s show hyperacute T-waves at time = 0h and then 2h later as they develop into STE.
- when in 2 contiguous leads, these may be an early sign of developing infarct/STE. They are broad, asymmetric and have a more gradual upstroke than downstroke.
- Serial ECG’s are critical.
Documentation
It may be worthwhile to develop a macro that documents all of these on an ECG (as long as we are actually looking for it).
This ECG does not show any signs of occlusion MI:
- there are no ST elevations in contiguous leads
- no de Winters waves (↓ST + peaked T's)
- no Wellens A: biphasic T's in V2/V3
- no Wellens B: deep symmetrical T-wave inversions in V2/V3
- no hyperacute T waves
- no signs of posterior or right sided MIOur best tool to diagnose occlusion MI is the ECG. How well does this perform?
| ECG marker | sensitivity for occlusion MI |
|---|---|
| subtle STE | 83% |
| reciprocal STD or negative hyper acute T | 82% |
| terminal QRS distortion = J-point 50% of the R – wave | 53% |
| inf STE with hi lat reciprocal changes (STD/TWI in aVL) | 50% |
| hyperacute TW | 49% |
| STD max in V1-V4 | 45% |
| acute pathological Q waves | 47% |
Remembering that our goal is a <2% miss rate for 30-day MACE, we need to supplement the ECG’s with troponin and history.
References
- Bivens, Matt MD. “STEMI Critics Are Right. We’re Missing Too Many Heart Attacks.” Emergency Medicine News 47(3):p 2,11,15, April 2025. | DOI: 10.1097/01.EEM.0000000000000015. Accessed 21 April 2025. https://journals.lww.com/em-news/fulltext/2025/04000/stemi_critics_are_right__we_re_missing_too_many.3.aspx
You must be logged in to post a comment.